INFORMATION
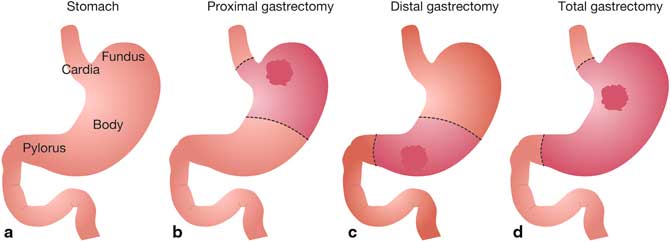
Gastrectomy
Gastrectomy is surgery to remove part or all of the stomach.
- If only part of the stomach is removed, it is called partial gastrectomy
- If the whole stomach is removed, it is called total gastrectomy
Description
The surgery is done while you are under general anesthesia (asleep and pain free). The surgeon makes a cut in the abdomen and removes all or part of the stomach, depending on the reason for the procedure.
Depending on what part of the stomach was removed, the intestine may need to be reconnected to the remaining stomach (partial gastrectomy) or to the esophagus (total gastrectomy).
Today, some surgeons perform gastrectomy using a camera. The surgery, which is called laparoscopy is done with a few small surgical cuts. The advantages of this surgery are a faster recovery, less pain, and only a few small cuts.
Why the Procedure is Performed
This surgery is used to treat stomach problems such as:
- Bleeding
- Inflammation
- Cancer
- Polyps (growth on the lining of the stomach)
Risks
Risks for anesthesia and surgery in general include:
- Reactions to medicines or breathing problems
- Bleeding, blood clots, or infection
Risks for this surgery include:
- Leak from connection to the intestine which can cause infection or abscess
- The connection to the intestine narrows, causing blockage
Before the Procedure
If you are a smoker, you should stop smoking several weeks before surgery and not start smoking again after surgery. Smoking slows recovery and increases the risk of problems. Tell your health care provider if you need help quitting.
Tell your surgeon:
- If you are or might be pregnant
- What medicines, vitamins, herbs, and other supplements you are taking, even ones you bought without a prescription
During the week before your surgery:
- You may be asked to stop taking blood thinners. These include NSAIDs (aspirin, ibuprofen), vitamin E, warfarin (Coumadin), dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis), and clopidegrel (Plavix).
- Ask your surgeon which drugs you should still take on the day of your surgery.
- Prepare your home for when you go home after surgery. Set up your home to make your life easier and safer when you return.
On the day of your surgery:
- Follow instructions about not eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
You may stay in hospital for 6 to10 days.
After surgery, there may be a tube in your nose which will help keep your stomach empty. It is removed as soon as your bowels are working well.
Most people have pain from the surgery. You may receive a single medicine or a combination of medicines to control your pain. Tell your providers when you are having pain and if the medicines you are receiving control your pain.
How well you do after surgery depends on the reason for the surgery and your condition.
Ask your surgeon if there are any activities you shouldn’t do after you go home. It may take several weeks for you to recover fully. While you are taking narcotic pain medicines, you should not drive.
Your Recovery
You will have some belly pain and may need pain medicine for the first week or so after surgery. The cut that the doctor made (incision) may be tender and sore.
Because the surgery makes your stomach smaller, you will get full more quickly when you eat. Food also may empty into the small intestine too quickly. This is called dumping syndrome. It can cause diarrhea and make you feel faint, shaky, and nauseated. It also can make it hard for your body to get enough nutrition. If you think you are having problems with dumping syndrome, talk to your doctor.
It is important to avoid heavy lifting or strenuous exercise while you are recovering so that your belly can heal. You will probably be able to return to work or your normal routine in 4 to 6 weeks.
This care sheet gives you a general idea about how long it will take for you to recover. But each person recovers at a different pace. Follow the steps below to get better as quickly as possible.
How can you care for yourself at home?
- Rest when you feel tired. Getting enough sleep will help you recover.
- Try to walk each day. Start out by walking a little more than you did the day before. Bit by bit, increase the amount you walk. Walking boosts blood flow and helps prevent pneumonia and constipation.
- Avoid lifting anything that would make you strain. This may include heavy grocery bags and milk containers, a heavy briefcase or backpack, cat litter or dog food bags, a vacuum cleaner, or a child.
- Avoid strenuous activities, such as bicycle riding, jogging, weight lifting, or aerobic exercise, until your doctor says it is okay.
- Do not take part in any activity where you could be hit in the belly. This could be sports or playing with children.
- Hold a pillow over your incision when you cough or take deep breaths. This will support your belly and decrease your pain.
- Do breathing exercises at home as instructed by your doctor. This will help prevent pneumonia.
- You can shower. Pat the incision dry. Do not take a bath for the first 2 weeks, or until your doctor tells you it is okay.
- Ask your doctor when you can drive again.
- You will probably need to take 4 to 6 weeks off from work. It depends on the type of work you do and how you feel.
- Ask your doctor when it is okay for you to have sex.
Call your doctor or nurse call line now if :
- You are sick to your stomach or cannot keep fluids down.
- You have pain that does not get better after you take pain medicine.
- You have signs of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the wound.
- Pus draining from the wound.
- A fever.
- You have loose stitches, or your incision comes open.
- You have signs of a blood clot in your leg (called a deep vein thrombosis), such as:
- Pain in your calf, back of the knee, thigh, or groin.
- Redness and swelling in your leg or groin.
- You cannot pass stool or gas.
- Bright red blood has soaked through your bandage.
Watch closely for any changes in your health and be sure to contact your doctor or nurse call line if you have any problems.
How do you eat after a gastrectomy?
Eat smaller meals five to six times a day.
- Your stomach cannot hold as much food after surgery.
- Eat no more than one cup of food at each meal or snack.
- Add new foods slowly to lower side effects of dumping syndrome.
- Chew food really well.
CONCLUSION
All the Lorem Ipsum generators on the Internet tend to repeat predefined chunks as necessary, making this the first true generator on the Internet. It uses a dictionary of over 200 Latin words, combined with a handful of model sentence structures, to generate Lorem Ipsum which looks reasonable.