INFORMATION
HIATAL HERNIA- ANTI-REFLUX SURGERY
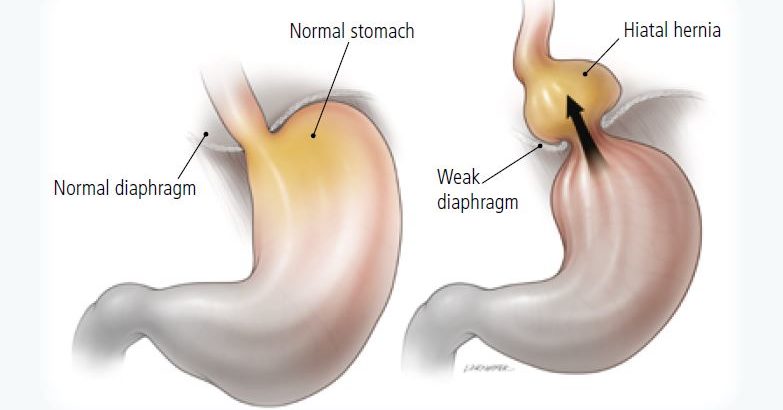
A hiatal hernia is a condition in which the upper part of your stomach bulges through an opening in your diaphragm. Your diaphragm is the thin muscle that separates your chest from your abdomen. Your diaphragm helps keep acid from coming up into your esophagus. When you have a hiatal hernia, it’s easier for the acid to come up. This leaking of acid from your stomach into your esophagus is called GERD (gastroesophageal reflux disease). GERD may cause symptoms such as
- Heartburn
- Problems swallowing
- A dry cough
- Bad breath
- Nausea and/or vomiting
- Breathing problems
- The wearing away of your teeth
Often, the cause of a hiatal hernia is unknown. It may have to do with weakness in the surrounding muscles. Sometimes the cause is an injury or a birth defect. Your risk of getting a hiatal hernia goes up as you age; they are common in people over age 50. You are also at higher risk if you have obesity or smoke.
WHEN IS SURGERY REQUIRED?
Most hiatal hernias do not cause symptoms, and therefore treatment is not usually necessary. Those who have mild symptoms, such as heartburn, acid reflux, or gastroesophageal reflux disorder (GERD) may be able to treat their condition with medications or lifestyle changes.However, surgery may be recommended if:
- symptoms are severe and interfere with quality of life
- symptoms do not respond to other treatments
- the hernia is at risk of becoming strangulated, which is where the blood supply to the herniated tissue is cut off — a situation that can be fatal
- symptoms include bleeding, ulcers, or narrowing of the food pipe (esophagus), which is known as an esophageal stricture
WHAT TYPES OF SURGERY ARE THERE?
There are three types of surgery for a hiatal hernia: Nissen fundoplication (keyhole surgery), open repairs, and endoluminal fundoplication. All three procedures require a general anesthetic.
Exams and Tests
Tests that may be used include:
- Barium swallow x-ray
- Esophagogastroduodenoscopy ( EGD)
TREATMENT
The goals of treatment are to relieve symptoms and prevent complications. Treatments may include:
- Medicines to control stomach acid
- Surgery to repair the hiatal hernia and prevent reflux
Other measures to reduce symptoms include:
- Avoiding large or heavy meals
- Not lying down or bending over right after a meal
- Reducing weight and not smoking
- Raising the head of the bed 4 to 6 inches (10 to 15 centimeters)
If medicines and lifestyle measures do not help control symptoms, you may need surgery.
SURGERY
Description
The most common procedure of this type is called fundoplication. In this surgery, your surgeon will:
- First repair the hiatal hernia, if one is present. This involves tightening the opening in your diaphragm with stitches to keep your stomach from bulging upward through the opening in the muscle wall. Some surgeons place a piece of mesh in the repaired area to make it more secure.
- Wrap the upper part of your stomach around the end of your esophagus with stitches. The stitches create pressure at the end of your esophagus, which helps prevent stomach acid and food from flowing up from the stomach into the esophagus.
Surgery is done while you are under general anesthesia, so you are asleep and pain-free. Surgery most often takes 2 to 3 hours. Your surgeon may choose from different techniques.
OPEN REPAIR
- Your surgeon will make 1 large surgical cut in your belly.
- A tube may be inserted into your stomach through the abdomen to keep the stomach wall in place. This tube will be taken out in about a week.
LAPAROSCOPIC REPAIR
- Your surgeon will make 3 to 5 small cuts in your belly. A thin tube with a tiny camera on the end is inserted through one of these cuts.
- Surgical tools are inserted through the other cuts. The laparoscope is connected to a video monitor in the operating room.
- Your surgeon does the repair while viewing the inside of your belly on the monitor.
- The surgeon may need to switch to an open procedure in case of problems.
ENDOLUMINAL FUNDOPLICATION
- This is a new procedure that can be done without making cuts. A special camera on a flexible tool (endoscope) is passed down through your mouth and into your esophagus.
- Using this tool, the doctor will put small clips in place at the point where the esophagus meets the stomach. These clips help prevent food or stomach acid from backing up.
RECOVERY TIME
After laparoscopic surgery, most people will not experience much pain, but they may feel discomfort in their abdomen and chest and have difficulty swallowing. This usually passes within 48 hours.
After a laparoscopy, a person may be able to go home the same day if they have recovered from the anesthetic. Otherwise, they may spend a night in the hospital and should be able to walk around the day after the surgery.
A person may soon feel well again but may find that they tire easily.
In the days after surgery, a person will usually be advised to:
- wash the incision area daily with plain soap and water
- shower instead of bathing, and avoid the use of pools and hot tubs
- walk about when possible to stop blood clots from forming in the leg
- avoid drinking through a straw
- practice specific breathing and coughing exercises to strengthen the diaphragm
In the weeks after surgery is recommend the following:
- avoiding any heavy lifting for 2 to 3 weeks
- avoiding driving for 7 to 10 days
- returning to work within 2 to 3 weeks, or whenever a person is feeling well enough
- taking painkillers for several days after surgery to minimize discomfort
A person will need to follow a specific diet after surgery. It is advisable to drink clear liquids immediately after surgery and move onto soft or liquefied foods, including mashed potatoes, smoothies, and soups, the following day. A person should also avoid foods that cause gas and bloating.
During recovery, it might be a good idea for people to eat several smaller meals throughout the day instead of three large ones.
Most people can return to their regular diet between 3 to 6 weeks after surgery.
However, even after a person makes a full recovery, their doctor may recommend they continue to limit or avoid foods that contribute to gas, bloating, and acid reflux symptoms, such as:
- acidic foods, including citrus fruits and tomato products
- alcohol
- beans and lentils
- carbonated beverages
- corn
- cruciferous vegetables, including broccoli, cabbage, and cauliflower
Open surgery will usually require a lengthier stay in the hospital and an extended recovery time.
Risks
Risks of any anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots, or infections
Risks of this surgery are:
- Damage to the stomach, esophagus, liver, or small intestine. This is very rare.
- Gas bloat. This is when the stomach overfills with air or food and you are unable to relieve the pressure by burping or vomiting. These symptoms slowly get better for most people.
- Pain and difficulty when you swallow. This is called dysphagia. In most people, this goes away during the first 3 months after surgery.
- Return of the hiatal hernia or reflux.
Outlook (Prognosis)
Heartburn and other symptoms should improve after surgery. Some people still need to take drugs for heartburn after surgery.
You may need another surgery in the future if you develop new reflux symptoms or swallowing problems. This may happen if the stomach was wrapped around the esophagus too tightly, the wrap loosens, or a new hiatal hernia develops.