INFORMATION
Ileostomy
An ileostomy is used to move waste out of the body. This surgery is done when the colon or rectum is not working properly.
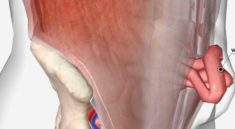
The word “ileostomy” comes from the words “ileum” and “stoma.” Your ileum is the lowest part of your small intestine. “Stoma” means “opening.” To make an ileostomy the surgeon makes an opening in your belly wall and brings the end of the ileum through the opening. The ileum is then attached to the skin.
Description
Before you have surgery to create an ileostomy, you may have surgery to remove all of your colon and rectum, or just part of your small intestine.
These surgeries include:
- Small bowel resection
- Total abdominal colectomy
- Total proctolocolectomy
An ileostomy may be used for a short or long time.
When your ileostomy is temporary, it most often means all of your large intestine was removed. However, you still have at least part of your rectum. If you have surgery on part of your large intestine, your health care provider may want the remainder of your intestine to rest for a while. You will use the ileostomy while you recover from this surgery. When you do not need it anymore, you will have another surgery. This surgery will be done to reattach the ends of the small intestine. You will no longer need the ileostomy after this.
You will need to use it long-term if all of your large intestine and rectum have been removed.
To create the ileostomy, the surgeon makes a small surgical cut in the wall of your belly. Part of your small intestine that is farthest from your stomach is brought up and used to make an opening. This is called a stoma. When you look at your stoma, you are actually looking at the lining of your intestine. It looks a lot like the inside of your cheek.
Sometimes, an ileostomy is done as the first step in forming an ileal anal reservoir (called a J-pouch).
Why the Procedure is Performed
Ileostomy is done when problems with your large intestine can only be treated with surgery.
There are many problems that may lead to the need for this surgery. Some are:
- Inflammatory bowel disease (ulcerative colitis or Crohn disease). This is the most common reason for this surgery.
- Colon or rectal cancer
- Familial polyposis
- Birth defects that involve your intestines
- An accident that damages your intestines or another intestinal emergency
Risks
Talk with your provider about these possible risks and complications.
Risks of anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots
- Infection
Risks of this surgery are:
- Bleeding inside your belly
- Damage to nearby organs
- Dehydration (not having enough fluid in your body) if there is a lot of watery drainage from your ileostomy
- Difficulty absorbing needed nutrients from food
- Infection, including in the lungs, urinary tract, or belly
- Poor healing of the wound in your perineum (if your rectum was removed)
- Scar tissue in your belly that causes a blockage of the small intestine
- Wound breaking open
Before the Procedure
Always tell your provider what medicines you are taking, even medicines, supplements, or herbs you bought without a prescription.
Before your surgery, talk with your provider about the following things:
- Intimacy and sexuality
- Pregnancy
- Sports
- Work
During the 2 weeks before your surgery:
- Two weeks before surgery, you may be asked to stop taking drugs that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), Naprosyn (Aleve, Naproxen), and others.
- Ask your provider which drugs you should still take on the day of your surgery.
- If you smoke, try to stop. Ask your provider for help.
- Always let your provider know about any cold, flu, fever, herpes breakout, or other illness you may have before your surgery.
The day before your surgery:
- You may be asked to drink only clear liquids such as broth, clear juice, and water after some point.
- Your provider will tell you when to stop eating and drinking.
- Your provider may ask you to use enemas or laxatives to clear out your intestines.
On the day of your surgery:
- Take the drugs you were told to take with a small sip of water.
- You will be told when to arrive at the hospital.
After the Procedure
You will be in the hospital for 3 to 7 days. You may have to stay longer if your ileostomy was an emergency operation.
You may be able to suck on ice chips on the same day as your surgery to ease your thirst. By the next day, you will probably be allowed to drink clear liquids. You will slowly add thicker fluids and then soft foods to your diet as your bowels begin to work again. You may be eating again 2 days after your surgery.
Outlook (Prognosis)
Most people who have an ileostomy are able to do most of the activities they were doing before their surgery. This includes most sports, travel, gardening, hiking, and other outdoor activities, and most types of work.
If you have a chronic condition, such as Crohn disease or ulcerative colitis, you may need ongoing medical treatment.
What to Expect at Home
Your stoma is made from the lining of your intestine. It will be pink or red, moist, and a little shiny.
Stool that comes from your ileostomy is thin or thick liquid, or it may be pasty. It is not solid like the stool that comes from your colon. Foods you eat, medicines you take, and other things may change how thin or thick your stool is.
Some amount of gas is normal.
You will need to empty the pouch 5 to 8 times a day.
Self-care
Ask your health care provider what you should be eating when you are discharged from the hospital. You may be asked to follow a. low-residue diet.
Talk with your provider if you have diabetes, heart disease, or any other condition, and you need to eat or avoid certain foods.
You may take a bath or a shower as air, soap, and water will not hurt your stoma and water will not go into the stoma. It is okay to do this with or without your pouch on.
Drugs and medicines:
- Liquid medicines may work better than solid ones. Take these when they are available.
- Some drugs have a special (enteric) coating. Your body will not absorb these well. Ask your provider or pharmacist for other kinds of medicine.
Talk with your provider if you are taking birth control pills. Your body may not absorb them well enough to keep you from getting pregnant.
Ileostomy – changing your pouch
You had an injury or disease in your digestive system and needed an operation called an ileostomy. The operation changed the way your body gets rid of waste (stool, feces, or poop).
Now you have an opening called a stoma in your belly. Waste will pass through the stoma into a pouch that collects it. You will need to take care of the stoma and empty the pouch many times a day.
When to Change Your Pouch
Change your pouch every 5 to 8 days. If you have itching or leakage, change it right away.
If you have a pouch system made of 2 pieces (a pouch and a wafer) you can use 2 different pouches during the week. Wash and rinse the pouch not being used, and let it dry well.
Choose a time of day when there is less stool output from your stoma. Early in the morning before you eat or drink anything (or at least 1 hour after a meal) is best.
You may need to change your pouch more often if:
- You have been sweating more than usual from hot weather or exercise.
- You have oily skin.
- Your stool output is more watery than usual.
When to Call the Doctor
Call your provider if:
- Your stoma is swelling and is more than a half inch (1 centimeter) larger than normal.
- Your stoma is pulling in, below the skin level.
- Your stoma is bleeding more than normal.
- Your stoma has turned purple, black, or white.
- Your stoma is leaking often.
- Your stoma does not seem to fit as well as it did before.
- You have a skin rash, or the skin around your stoma is raw.
- You have a discharge from the stoma that smells bad.
- Your skin around your stoma is pushing out.
- You have any kind of sore on the skin around your stoma.
- You have any signs of being dehydrated (there is not enough water in your body). Some signs are dry mouth, urinating less often, and feeling lightheaded or weak.
- You have diarrhea that is not going away.
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only — they do not constitute endorsements of those other sites.