INFORMATION
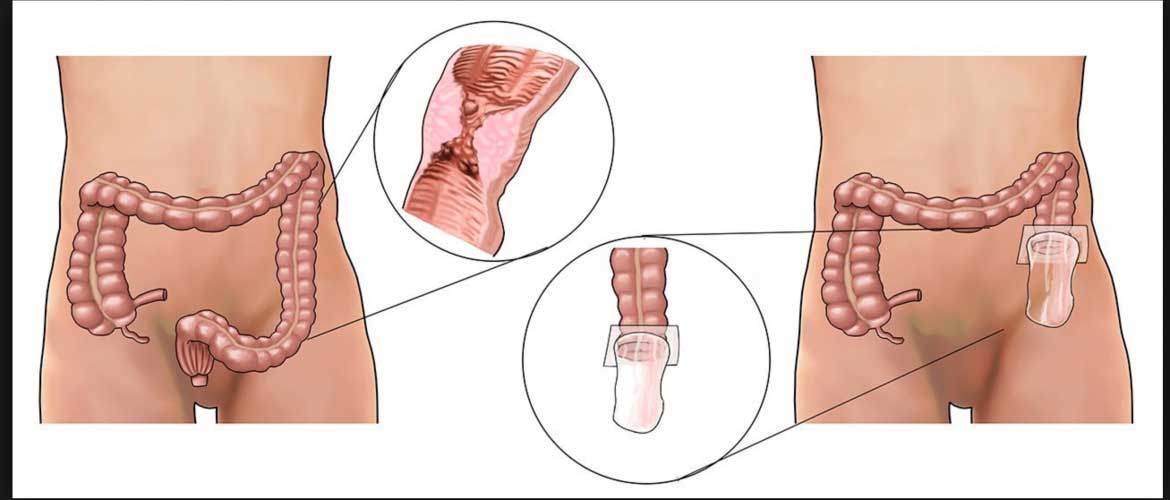
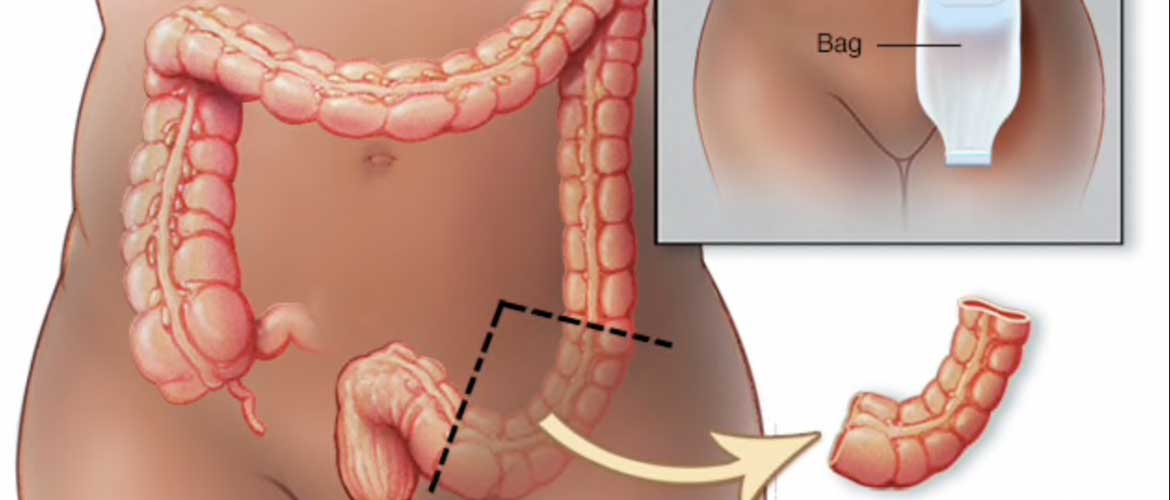
Colostomy is a surgical procedure that brings one end of the large intestine out through an opening (stoma) made in the abdominal wall. Stools moving through the intestine drain through the stoma into a bag attached to the abdomen.
Description
The procedure is usually done after:
- Bowel resection
- Injury to the bowel
The colostomy may be short-term or permanent.
Colostomy is done while you are under general anesthesia (asleep and pain-free). It may be done either with a large surgical cut in the abdomen or with a small camera and several small cuts (laparoscopy).
The type of approach used depends on what other procedure needs to be done. The surgical cut is usually made in the middle of the abdomen. The bowel resection or repair is done as needed.
For the colostomy, one end of the healthy colon is brought out through an opening made in the abdomen wall, usually on the left side. The edges of bowel are stitched to the skin of opening. This opening is called a stoma. A bag called a stoma appliance is placed around the opening to allow stool to drain.
Your colostomy may be short-term. If you have surgery on part of your large intestine, a colostomy allows the other part of your intestine to rest while you recover. Once your body has fully recovered from the first surgery, you will have another surgery to reattach the ends of the large intestine. This is usually done after 12 weeks.
Why the Procedure is Performed
Reasons a colostomy is done include:
- Infection of the abdomen, such as perforated diverticulitis or an abscess.
- Injury to the colon or rectum (for example, a gunshot wound).
- Partial or complete blockage of the large bowel (intestinal obstruction).
- Rectal or colon cancer
- Wounds or fistulas in the perineum. The area between the anus and vulva (women) or the anus and scrotum (men).
After the Procedure
You will be in the hospital for 3 to 7 days. You may have to stay longer if your colostomy was done as an emergency procedure.
You will be allowed to slowly go back to your normal diet:
- The same day as your surgery, you may be able to suck on ice chips to ease your thirst.
- By the next day, you will probably be allowed to drink clear liquids.
- Thicker fluids and then soft foods will be added as your bowels begin to work again. You may be eating normally within 2 days after surgery.
The colostomy drains stool (feces) from the colon into the colostomy bag. Colostomy stool is often softer and more liquid than stool that is passed normally. The texture of stool depends on which part of the intestine was used to form the colostomy.
Outlook (Prognosis)
Before you are released from the hospital, an ostomy nurse will teach you about diet and how to care for your colostomy.
What to Expect at Home
You may have these problems after you return home from the hospital:
- Pain when you cough, sneeze, and make sudden movements. This may last up to several weeks.
- Hard stools, or you may not be able to have a bowel movement at all.
- You may have diarrhea.
- You may have problems with your colostomy.
Activity:
- It may take several weeks for you to get back to your normal activities. Ask your provider if there are activities you should not do.
- Start by taking short walks.
- Increase your activity slowly. DO NOT push yourself too hard.
Your provider will give you pain medicines to take at home.
- If you are taking pain medicines 3 or 4 times a day, take them at the same times each day for 3 to 4 days. They control pain better this way.
- DO NOT drive or use other heavy machines if you are taking narcotic pain medicines. These medicines may make you drowsy and slow your reaction time.
Press a pillow over your incision when you need to cough or sneeze. This helps ease pain.
Ask your provider when you should start taking your regular medicines again after surgery.
Wound Care
If your staples or sutures have been removed, you will probably have small pieces of tape placed across your incision. These pieces of tape will fall off on their own. If your incision was closed with dissolving suture, you may have glue covering the incision. This glue will loosen and come off on its own. Or, it can be peeled off after a few weeks.
Ask your provider when you can shower or soak in a bathtub.
- It is OK if the tapes get wet. DO NOT soak or scrub them.
- Keep your wound dry at all other times.
- The tapes will fall off on their own after a week or two.
If you have a dressing, your provider will tell you how often to change it and when you can stop using it.
- Follow instructions for cleaning your wound daily with soap and water. Look carefully for any changes to the wound as you do this.
- Pat your wound dry. DO NOT rub it dry.
- Ask your provider before putting any lotion, cream, or herbal remedy on your wound.
DO NOT wear tight clothing that rubs against your wound while it is healing. Use a thin gauze pad over it to protect it if needed.
Sitting on a pillow may make you more comfortable if the surgery was in your rectum.
Diet
Eat small amounts of food several times a day. DO NOT eat 3 big meals.
- Space out your small meals.
- Add new foods back into your diet slowly.
- Try to eat protein every day.
Some foods may cause gas, loose stools, or constipation as you recover. Avoid foods that cause problems.
If you become sick to your stomach or have diarrhea, call your provider.
Ask your provider how much fluids you should drink each day to prevent getting dehydrated.
If you have hard stools:
- Try to get up and walk around more. Being more active can help.
- If you can, take less of the pain medicine your provider gave you. They can make you constipated. If OK with your provider, try using acetaminophen (Tylenol) or ibuprofen (Advil or Motrin) to help with pain.
- You may use stool softeners if your doctor tells you it is OK.
- Ask your provider if you can take milk of magnesia or magnesium citrate. DO NOT take any laxatives without asking your provider first.
- Ask the provider if it is OK to eat foods that contain a lot of fiber or take any over-the-counter fiber product such as psyllium (Metamucil).
Returning to Work
Return to work only when you feel ready. These tips may help:
- You may be ready when you can be active around the house for 8 hours and still feel OK when you wake up the next morning.
- You may want to start back part-time and on light duty at first.
- Your provider can write a letter to limit your work activities if you do heavy labor.
When to Call the Doctor
Call your provider if you have any of the following:
- Fever of 101°F (38.3°C) or higher, or you have a fever that does not go away with acetaminophen (Tylenol)
- Swollen belly
- Feel sick to your stomach or you are throwing up a lot
- Not had a bowel movement 4 days after leaving the hospital
- Have been having bowel movements and they suddenly stop
- Black or tarry stools, or there is blood in your stools
- Belly pain that is getting worse, and pain medicine does not help
- Shortness of breath or chest pain
- Swelling in the legs or pain in your calves
- Changes in your incision, such as the edges are pulling apart, drainage or bleeding coming from it, redness, warmth, or worsening pain
- Increased drainage from your rectum
NOTE: The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only — they do not constitute endorsements of those other sites.
psum.
CONCLUSION
All the Lorem Ipsum generators on the Internet tend to repeat predefined chunks as necessary, making this the first true generator on the Internet. It uses a dictionary of over 200 Latin words, combined with a handful of model sentence structures, to generate Lorem Ipsum which looks reasonable.